TL; DR: It's time for medical doctors to acknowledge the insights of microbiome science, and the impact of industrialized diets on gut permeability. As gastroenterologists, we can take the lead in emphasizing gut barrier health with our patients.
Balancing motherhood and professional growth is a tricky act, especially when it involves attending conferences. It's a whirlwind of learning, networking, and trying to stay at the top of your game, all while ensuring your family life doesn’t miss a beat (thank heavens for my amazing husband - his words, not mine 😉).
Recently, I found myself at a scientific conference in Washington D.C., eager to dive into the world of gut microbiota and its role in digestive health. Sponsored by the esteemed American Gastroenterological Association, I expected to be surrounded by the latest GI wellness products for common issues like dyspepsia, bloating, and diarrhea - essential tools for those of us living with and seeing patients with irritable bowel syndrome. Secretly, I also looked forward to a leisurely jog around the Tidal Basin among the cherry blossoms. After all, who says a mom can't enjoy a little getaway?
Imagine my surprise when “non-prescriptive” microbial therapeutics product displays were nowhere in sight at the conference. With the recent strides in microbial therapies for diseases like C. difficile colitis (i.e. such as with Reybota and Vowst for Clostridium Difficile Colitis), I assumed wellness innovations would be abundant. Yet, when it came to discussions of non-prescriptive microbial therapeutics for optimizing gut wellness or even for conditions like irritable bowel syndrome, this was not on the agenda.
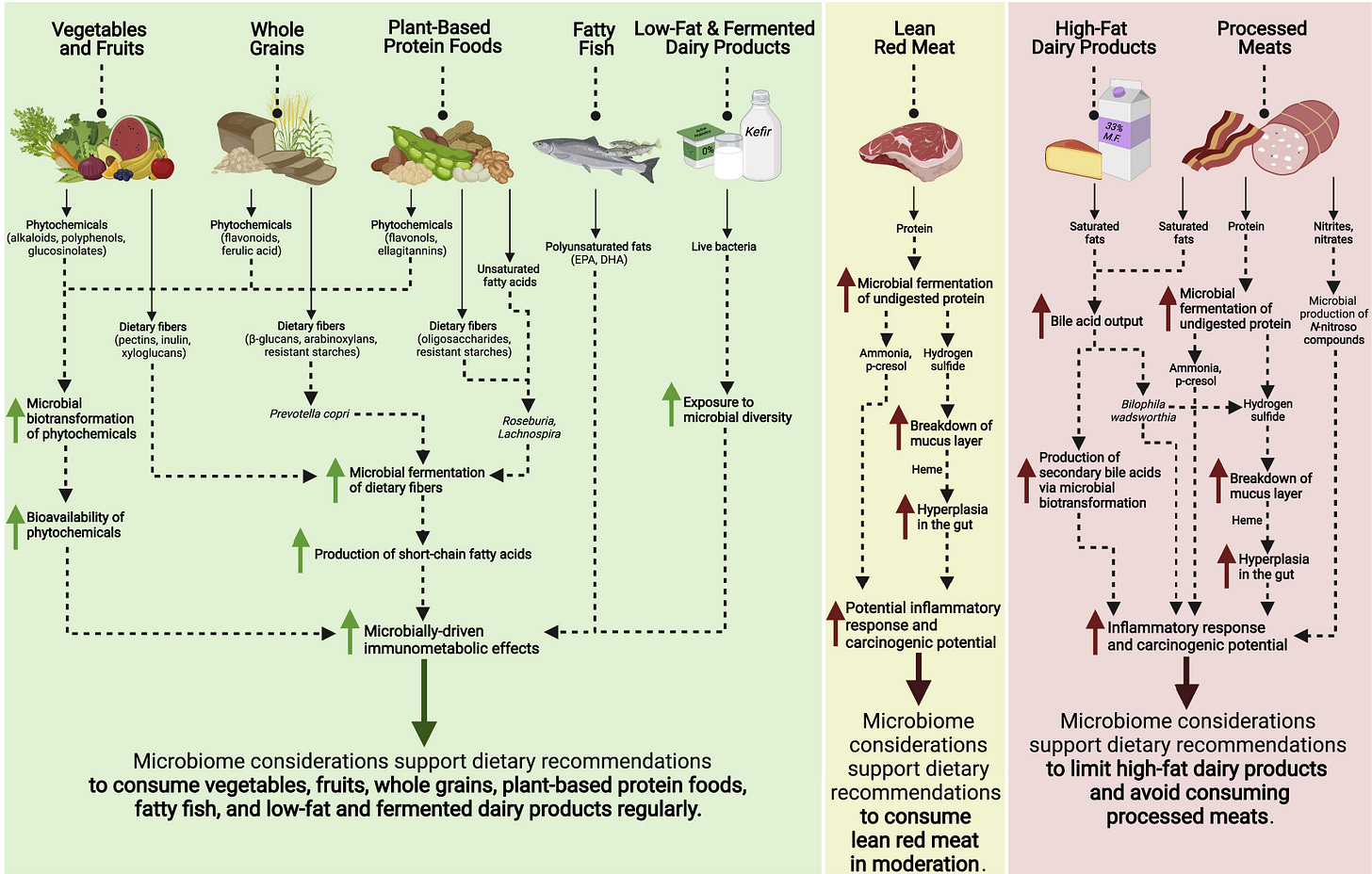
Worldwide, nutritional guidelines do not mention or even consider the gut microbiota.1
Despite my initial letdown, a cascade of scientific presentations profoundly shifted my perspective and approach to medicine. The recurring theme was clear: our modern, industrialized diets are compromising our gut barrier, leading to inflammation and chronic diseases - even among the outwardly healthy.
The scientific presentation also prompted me to reconsider how we study gut microbes. Most research relies on samples from the large intestine, leaving the small intestine - a critical site of digestion and microbial residence - largely unexplored due to the practical challenges of sampling. While more research is being done on the small bowel microbiota, I wondered about the accuracy of this information?
The Mediterranean Diet alters the gut microbiota in a beneficial way that reduces subclinical gut inflammation in otherwise healthy individuals.2
During the event, I bonded with another private practice lady gastroenterologist. Over lunch, we shared a moment, reflecting on the misguidance we may have offered patients regarding gut permeability, once thought to be exclusive to severe disease states like inflammatory bowel disease. We exchanged rueful smiles that conveyed a silent apology for our unwitting ignorance.
A Conference Highlight
The conference's highlight was Dr. Jens Walter's keynote on the adverse effects of industrialized diets on the gut barrier.
Even well individuals on a typical Canadian diet displayed metabolic signs of subclinical gut inflammation and a microbiota capable of damaging the gut lining. Yet this microbiota and metabolic parameters much improved when the individuals went on a non-industrialized diet! Hope!
The contrast between modern diets (i.e. 17 grams of fiber per day) and those of our ancestors (i.e. 100 grams of dietary fiber per day) was striking.
The focus on that such extraordinary amounts of fiber could be so beneficial was particularly intriguing, given my clinical observations of fiber sometimes making irritable bowel syndrome worse. Could our industrialized diets have eroded our microbiota to the point where we can't tolerate the fiber levels of our ancestors?
The disconnect between nutritionists and microbiome experts is startling. National dietary guidelines across the globe fail to consider the gut microbiota's crucial role in our diet and overall health, a glaring omission that could explain the pervasive digestive discomfort many of us experience.
Check out the right column →High fat dairy products create a bloom of Bilophila breaking down the gut barrier’s mucous layer inducing gut inflammation.1
Dietary fiber is substrate (food!) for the gut microbiota and helps the gut barrier make a healthy mucous layer. Avoid being ‘fiber starved’!1,3
In my practice, I have always emphasized addressing vitamin deficiencies and weight fluctuations linked to GI diseases, often diverging from my colleagues who might overlook these concerns. But I realize now that every patient interaction should have begun with the basics of GI wellness, starting with maintaining a healthy gut barrier.
This may come off as an apology, and in a way, it is. I had not been fully informed (thank you world experts on the gut microbiome!). I now see that everyday gut permeability is influenced by our industrialized way of life, and for that oversight, I am deeply sorry.
End dictation.
Your Lady MD,
Emily
References
1. Armet AM, Deehan EC, O'Sullivan AF, et al. Rethinking healthy eating in light of the gut microbiome. Cell Host Microbe. Jun 8 2022;30(6):764-785. doi:10.1016/j.chom.2022.04.016
2. Turpin W, Dong M, Sasson G, et al. Mediterranean-Like Dietary Pattern Associations With Gut Microbiome Composition and Subclinical Gastrointestinal Inflammation. Gastroenterology. Sep 2022;163(3):685-698. doi:10.1053/j.gastro.2022.05.037
3. Jones JM. CODEX-aligned dietary fiber definitions help to bridge the 'fiber gap'. Nutr J. Apr 12 2014;13:34. doi:10.1186/1475-2891-13-34






Love this!!